Meagan Piker has gotten a mammogram nearly every year for decades, and it’s not a comfortable affair.
“It entails essentially standing in a room in front of a really big machine, half-naked with a lead apron on, and then having your breasts smashed as flat as they can make them so that they can get a good image of the breast tissue,” she says. “And so it’s very uncomfortable. But it’s also, you know, it only takes 15 or 20 minutes and you’re done.”
She started getting mammograms at a young age because of a family history of breast cancer. Her grandmother passed away from it when she was just 40. And her mother was diagnosed at 43 and lived with it for over 20 years. She passed away a little over five years ago.
“So obviously, it’s always been a big presence in my life,” Piker says. “Thinking about it and hoping that I don’t follow the family tradition of getting breast cancer. And so far, knock on wood, I’ve been lucky.”
Mammograms can detect lumps or tumors two to three years before a primary care provider can feel them, and those who regularly screen see breast cancer death rates decrease by about 25 percent. Piker knows why mammograms matter. But others without that family history or genetic disposition wait for much longer. And in the age of COVID-19, they’re waiting too long. That’s according to Dr. Joshua Ofman, Chief Medical Officer at GRAIL, a healthcare company whose mission is to detect cancers early.
“People have just stopped getting their screening tests and stopped going to their doctors,” Ofman says. “And it’s for many, many reasons. Some health systems and doctors’ offices stopped offering those tests. And then others are really afraid to go to their doctor’s office in their hospital for fear of getting infected. So it’s a terrible confluence of issues, and it’s really tragic to see because the National Cancer Institute is now saying that the cancer death rate is going to increase as a result of this.”
Regular cancer screenings have declined by between 60 and 80 percent nationwide since the start of the COVID-19 pandemic. And according to The American Cancer Institute, nearly 10,000 additional patients will pass away from just two cancer types (breast and colorectal) over the next decade because of missed or delayed screenings during COVID-19. Dr. Ofman says cancer could soon become the leading cause of death in the world.
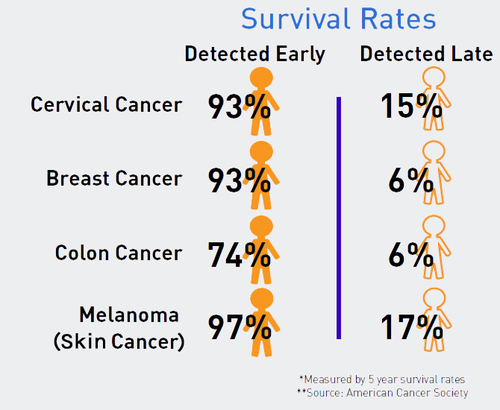
Early detection of abnormal tissue in a smaller surface area increases the treatment options for several major cancers, and thus reduces the chance of death, according to the American Cancer Institute. (Screenshot)
“We’re losing about 1,700 loved ones every day to cancer in this country,” he says. “And the reason is because we’re detecting most cancers too late when they’re already spread, and the outcomes are poor and treatments are less effective. And so the reason there’s been a focus on cancer screening is because it’s known that, if we can find cancer early, about nine in 10 people will survive five or more years. Whereas, if you find cancer late after it’s spread, only two out of 10 people will survive five or more years.”
That’s why Ofman is on a public relations mission to get more people to their doctor to get screenings for breast, colon, prostate, and other cancers, especially if you’re over 50 or have a family history. Dr. Eric Wieman is a surgeon at St. John’s Medical Center in Jackson, and he manages many colonoscopies and other cancer screenings. He agrees that it’s important for people to get their regular checkups.
“If you’re a high risk-person and you’ve been holding your colonoscopy since March. You know, it’s December,” Wieman says. “That’s nine months you’re behind. And, you know, that’s a long time for a person who has a history of developing an aggressive tumor to not do this screen.”
Dr. Wieman says that, like the rest of the U.S., St. John’s is likely to see a spike in late and advanced-stage cancers. Not only will that tragically cause more deaths, it also means more uncomfortable treatments for patients.
“Let’s say that instead of finding a colon cancer patient with a polyp that is removed and that doesn’t require surgery, maybe we find a larger colon cancer with some regional lymph nodes involved and the patient does have to undergo surgery to have this cancer removed,” he says. “That patient may overall have the same mortality. They live the same length of their life. But the procedures involved and the treatment is probably more complicated because they have a more advanced cancer.”
That means more money, more discomfort, and less time with family. The same could be said for other elective, noncancerous procedures, which have also seen declines. A hernia that requires a simple removal in March could mean a lost ski season this Winter. Dr. Wieman understands why people are wary of seeing their doctor, but he says St. John’s is taking every necessary precaution to protect people from the Coronavirus.
“Everybody at St. John’s put a lot of time and thought into taking good care of our patients and making sure that these procedures are safe during the pandemic,” he says. “Everybody wears a mask. Social distancing is enforced.”
After an initially huge drop-off of cancer screenings during March and April, numbers in Teton County have slowly improved. However, Wieman isn’t quite sure what will happen at the end of this year, when he typically sees an uptick in elective procedures. It’s especially up in the air since COVID is spiking locally and nationally, but Wieman reminds people that cancer detection, diagnoses, and incident rates are unlikely to change despite a raging pandemic.
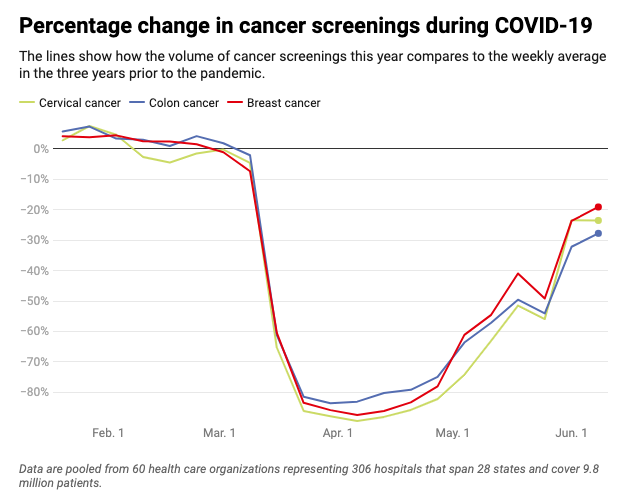
Cancer screening rates in the U.S. plummeted during March and April, but began to recover by the early summer. (Data by the Epic Health Research Network. Visualization by Time Magazine)
“Although the Coronavirus is a very devastating disease, it is not the worst disease,” Wieman says. “And we have to keep our cancer screenings going so that we cannot paralyze the medical system just because we have a pandemic. We have to compartmentalize the problem and keep things going.”
Meagan Piker agrees. She needs to wait a bit longer than usual for her yearly mammogram. But that doesn’t set her back too much, and she says people just need to be patient during a time when medical resources are strained.
“Everyone should try to get in to see their doctors as appropriate, but also try not to freak out if you have to wait a little bit longer,” Piker says. “I think we all just have to try to do our best during this really challenging time.”
It’s estimated that over 600,000 people will pass away from cancer in the U.S in 2020. That’s likely more than double the numbers for the Coronavirus. However, cancer death rates have steadily decreased since the 1990s, and new early detection methods are on the horizon.